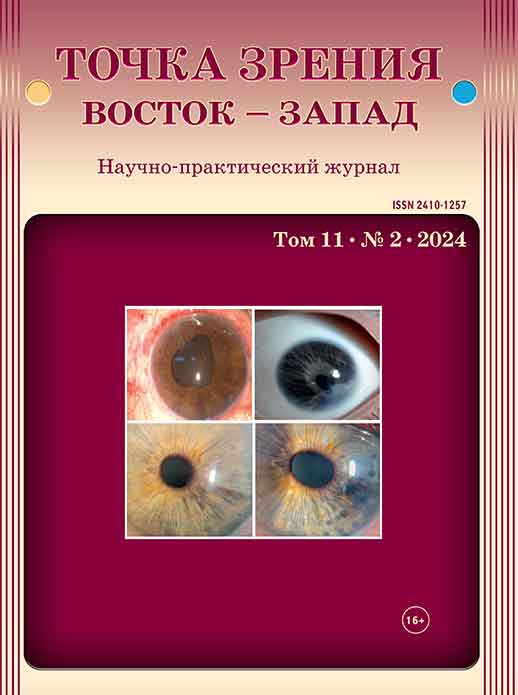
Некротизирующий энтероколит новорожденных как фактор риска развития ретинопатии недоношенных. Обзор литературы
Ключевые слова:
ретинопатия недоношенных, некротизирующий энтероколит, кишечный микробиом, фактор роста эндотелия сосудов, обзорАннотация
В данном обзоре литературы предлагаем рассмотреть некротизирующий энтероколит (НЭК) как фактор риска развития ретинопатии недоношенных (РН). РН, являясь одной из доминирующих причин слепоты и слабовидения среди детского населения, считается важной проблемой здравоохранения. Множество эпидемиологических исследований выявили значимую взаимосвязь между НЭК и развитием РН, наряду с неонатальным сепсисом, бронхолегочной дисплазией, внутрижелудочковыми кровоизлияниями и открытым артериальным протоком. В исследованиях отмечено, что пациенты с НЭК, требующие хирургического лечения, имеют меньший гестационный возраст и меньшую массу тела при рождении, а частота встречаемости РН у данной группы пациентов составляет 55%. Одним из возможных связующих звеньев между НЭК и РН выделяют воспалительный стресс, который приводит к аномальному развитию сосудов сетчатки и увеличению сосудистых анастомозов. Отдельно стоит выделить микробиом кишечника, который имеет множественные перекрестные связи с различными органами, в том числе способен оказывать влияние на орган зрения. Так, микробиом участвует в патогенезе НЭК и может оказывать влияние на РН посредством связи с экспрессией фактора роста эндотелия сосудов, усиливая выработку цитокинов, препятствуя реваскуляризации тканей и восстановлению сосудов. Еще одним связующим звеном между микробиомом и РН может быть влияние кишечной флоры на развитие неонатального сепсиса и бронхолегочной дисплазии, которые также выделяют как факторы риска РН. Однако исследования о влиянии пробиотиков на течение РН противоречивы и требуют дальнейшего изучения. Таким образом, НЭК можно рассматривать как один из факторов риска развития и прогрессирования РН.
Библиографические ссылки
1. Министерство здравоохранения Российской Федерации. Клинические рекомендации «Ретинопатия недоношенных». Доступно по: https://docs.google.com/viewerng/viewer?url=http://avoportal.ru/documents/fkr/fkr_rn_2023_.pdf [Ссылка активна на 17.03.2024] [Ministry of Health of the Russian Federation. Clinical guidelines «Retinopathy of prematurity». Available from: https://docs.google.com/viewerng/viewer?url=http://avoportal.ru/documents/fkr/fkr_rn_2023_.pdf [Accessed 17th march 2024] (In Russ.)]
2. Blencowe H, Moxon S, Gilbert C. Update on Blindness Due to Retinopathy of Prematurity Globally and in India. Indian Pediatr. 2016;53(2): 89–92.
3. Gilbert C. Retinopathy of prematurity: a global perspective of the epidemics, population of babies at risk and implications for control. Early Hum Dev. 2008 Feb;84(2): 77–82. doi: 10.1016/j.earlhumdev. 2007.11.009
4. Blencowe H, Lawn JE, Vazquez T, Fielder A, Gilbert C. Preterm–associated visual impairment and estimates of retinopathy of prematurity at regional and global levels for 2010. Pediatr Res. 2013 Dec;74(Suppl 1): 35–49. doi: 10.1038/pr.2013.205
5. Tandon M, Ranjan R, Muralidharan U, Kannan A. Influence of Anaemia on Multifactorial Disease Retinopathy of Prematurity: A Prospective Observational Study. Cureus. 2022;14(8): e27877. doi: 10.7759/cureus.27877
6. Gaber R, Sorour OA, Sharaf AF, Saad HA. Incidence and Risk Factors for Retinopathy of Prematurity (ROP) in Biggest Neonatal Intensive Care Unit in Itay Elbaroud City, Behera Province, Egypt. Clin Ophthalmol. 2021;15: 3467–3471. doi: 10.2147/OPTH.S324614
7. Макогон С.И., Горбачева Н.В., Хлопкова Ю.С. Преэклампсия как фактор риска развития ретинопатии недоношенных. Российская педиатрическая офтальмология. 2022;3: 39–44. [Makogon SI, Gorbacheva NV, Khlopkova YuS. Preeclampsia as a risk factor for the development of retinopathy of prematurity. Russian pediatric ophthalmology. 2022 3: 39–44. (In Russ)] doi: 10.17816/ rpoj109228
8. Opara CN, Akintorin M, Byrd A, Cirignani N, Akintorin S, Soyemi K. Maternal diabetes mellitus as an independent risk factor for clinically significant retinopathy of prematurity severity in neonates less than 1500g. PLoS One. 2020;15(8): e0236639. doi: 10.1371/ journal.pone.0236639
9. Yucel OE, Eraydin B, Niyaz L, Terzi O. Incidence and risk factors for retinopathy of prematurity in premature, extremely low birth weight and extremely low gestational age infants. BMC Ophthalmol. 2022;22(1): 367. doi: 10.1186/s12886-022-02591-9
10. Deb D, Annamalai R, Muthukumar M. Incidence, risk factors, progression, and involution in retinopathy of prematurity at a tertiary care center in South India. Oman J Ophthalmol. 2023;16(3): 452–460. doi: 10.4103/ojo.ojo_239_22
11. Yang J, Chen X, Liu T, Shi Y. Potential role of bile acids in the pathogenesis of necrotizing enterocolitis. Life Sci. 2024;336: 122279. doi: 10.1016/j.lfs.2023.122279
12. Kelleher ST, McMahon CJ, James A. Necrotizing Enterocolitis in Children with Congenital Heart Disease: A Literature Review. Pediatr Cardiol. 2021 Dec;42(8): 1688–1699. doi: 10.1007/s00246-021-02691-1
13. Alganabi M, Lee C, Bindi E, Li B, Pierro A. Recent advances in understanding necrotizing enterocolitis. F1000Res. 2019;8: F1000 Faculty Rev-107. doi: 10.12688/f1000research.17228.1
14. Neu J, Walker WA. Necrotizing enterocolitis. N Engl J Med. 2011;364(3): 255–264. doi: 10.1056/NEJMra1005408
15. Kelleher ST, Coleman J, McMahon CJ, James A. Outcomes and characteristics in term infants with necrotising enterocolitis and CHD. Cardiol Young. 2024;1: 7. doi: 10.1017/S1047951123004249
16. Сидоренко Е.И. Новая концепция патогенеза ретинопатии недоношенных. Российская детская офтальмология. 2020;3: 5–12. [Sidorenko EI. New concept of the pathogenesis of retinopathy of prematurity. Russian pediatric ophthalmology. 2020;3: 5–12. (In Russ.)] doi: 10.25276/2307-6658-2020-3-5-12
17. Woods J, Biswas S. Retinopathy of prematurity: from oxygen management to molecular manipulation. Mol Cell Pediatr. 2023;10(1): 12. doi: 10.1186/s40348-023-00163-5
Pammi M, Hollister E, Neu J. Gut Injury and the Microbiome in Neonates. Clin Perinatol. 2020;47(2): 369–382. doi: 10.1016/j. clp.2020.02.010
19. Stanikova A, Jouza M, Bohosova J, Slaby O, Jabandziev P. Role of the microbiome in pathophysiology of necrotising enterocolitis in preterm neonates. BMJ Paediatr Open. 2023;7(1): e002172. doi: 10.1136/bmjpo-2023-002172
20. Sampath V, Martinez M, Caplan M, Underwood MA, Cuna A. Necrotizing enterocolitis in premature infants-A defect in the brakes? Evidence from clinical and animal studies. Mucosal Immunol. 2023;16(2): 208–220. doi: 10.1016/j.mucimm.2023.02.002
21. Zhang C, Sherman MP, Prince LS, Bader D, Weitkamp JH, Slaughter JC, McElroy SJ. Paneth cell ablation in the presence of Klebsiella pneumoniae induces necrotizing enterocolitis (NEC)-like injury in the small intestine of immature mice. Dis Model Mech. 2012;5(4): 522–532. doi: 10.1242/dmm.009001
22. Molteni M, Gemma S, Rossetti C. The Role of Toll-Like Receptor 4 in Infectious and Noninfectious Inflammation. Mediators Inflamm. 2016;2016: 6978936. doi: 10.1155/2016/6978936
23. Hackam DJ, Sodhi CP. Bench to bedside – new insights into the pathogenesis of necrotizing enterocolitis. Nat Rev Gastroenterol Hepatol. 2022;19(7): 468–479. doi: 10.1038/s41575-022-00594-x
24. De Plaen IG. Inflammatory signaling in necrotizing enterocolitis. Clin Perinatol. 2013;40(1): 109–124. doi: 10.1016/j. clp.2012.12.008
25. Schnabl KL, Van Aerde JE, Thomson AB, Clandinin MT. Necrotizing enterocolitis: a multifactorial disease with no cure. World J Gastroenterol. 2008;14(14): 2142–2161. doi: 10.3748/wjg.14.2142
26. Watkins DJ, Besner GE. The role of the intestinal microcirculation in necrotizing enterocolitis. Semin Pediatr Surg. 2013;22(2): 83– 87. doi: 10.1053/j.sempedsurg.2013.01.004
27. Noor MS, Elbarbary M, Embabi SN, Zaki MA, Awad H, Al-Feky M. Screening and Risk Factors for Retinopathy of Prematurity in a Tertiary Care Hospital in Cairo, Egypt. Clin Ophthalmol. 2022;16: 3257–3267. doi: 10.2147/OPTH.S383493
28. Goldstein GP, Leonard SA, Kan P, Koo EB, Lee HC, Carmichael SL. Prenatal and postnatal inflammation-related risk factors for retinopathy of prematurity. J Perinatol. 2019;39(7): 964–973. doi: 10.1038/s41372-019-0357-2
29. Shemesh R, Strauss T, Zaslavsky-Paltiel I, Lerner-Geva L, Reichman B, Wygnanski-Jaffe T; Israel Neonatal Network. Perinatal and neonatal risk factors for retinopathy of prematurity in very low birthweight, very preterm twins: a population-based study. Eye (Lond). 2023; 4. doi: 10.1038/s41433-023-02801-8
30. Riddick R, Meilstrup A, Ansari MAY, Ware J, Zepponi D, Smith A, Sawaya D, Mungan N, Garg PM. Clinical and Growth Correlates of Retinopathy of Prematurity in Preterm infants with Surgical Necrotizing Enterocolitis and intestinal Perforation. Res Sq. 2023:rs.3.rs-3022247. doi: 10.21203/rs.3.rs-3022247/v1
31. Fundora JB, Binenbaum G, Tomlinson L, Yu Y, Ying GS, Maheshwari A, Donohue P. Association of Surgical Necrotizing Enterocolitis and Its Timing with Retinopathy of Prematurity. Am J Perinatol. 2023;40(11): 1178–1184. doi: 10.1055/s-0041-1733785
32. Tremblay S, Miloudi K, Chaychi S, Favret S, Binet F, Polosa A, Lachapelle P, Chemtob S, Sapieha P. Systemic inflammation perturbs developmental retinal angiogenesis and neuroretinal function. Invest Ophthalmol Vis Sci. 2013;54(13): 8125–8139. doi: 10.1167/iovs.13-12496
33. Hong HK, Lee HJ, Ko JH, Park JH, Park JY, Choi CW, Yoon CH, Ahn SJ, Park KH, Woo SJ, Oh JY. Neonatal systemic inflammation in rats alters retinal vessel development and simulates pathologic features of retinopathy of prematurity. J Neuroinflammation. 2014;11: 87. doi: 10.1186/1742-2094-11-87
34. Rzayev T, Celiker H, Aykut A, Cerit K, Koyuncuer A, Gucyetmez S, Ozdemir H, Memisoglu A, Bilgen H, Ozek E. Intestinal perforation after intravitreal low dose ranibizumab injection for the treatment of type 1 retinopathy of prematurity: A case report. Eur J Ophthalmol. 2023;33(4): NP70–NP74. doi: 10.1177/11206721221099249
35. Aziz M, Prince JM, Wang P. Gut microbiome and necrotizing enterocolitis: Understanding the connection to find a cure. Cell Host Microbe. 2022;30(5): 612–616. doi: 10.1016/j.chom.2022.04.003
36. Singh A, Mittal M. Neonatal microbiome – a brief review. J Matern Fetal Neonatal Med. 2020;33(22): 3841–3848. doi: 10.1080/14767058.2019.1583738
37. Tchirikov M, Schlabritz-Loutsevitch N, Maher J, Buchmann J, Naberezhnev Y, Winarno AS, Seliger G. Mid-trimester preterm premature rupture of membranes (PPROM): etiology, diagnosis, classification, international recommendations of treatment options and outcome. J Perinat Med. 2018;46(5): 465–488. doi: 10.1515/jpm-2017-0027
38. Jia J, Xun P, Wang X, He K, Tang Q, Zhang T, Wang Y, Tang W, Lu L, Yan W, Wang W, Hu T, Cai W. Impact of Postnatal Antibiotics and Parenteral Nutrition on the Gut Microbiota in Preterm Infants During Early Life. JPEN J Parenter Enteral Nutr. 2020;44(4): 639–654. doi: 10.1002/jpen.1695
39. Raba AA, O’Sullivan A, Miletin J. Pathogenesis of necrotising enterocolitis: The impact of the altered gut microbiota and antibiotic exposure in preterm infants. Acta Paediatr. 2021;110(2): 433–440. doi: 10.1111/apa.15559
40. La Rosa PS, Warner BB, Zhou Y, Weinstock GM, Sodergren E, Hall-Moore CM, Stevens HJ, Bennett WE Jr, Shaikh N, Linneman LA, Hoffmann JA, Hamvas A, Deych E, Shands BA, Shannon WD, Tarr PI. Patterned progression of bacterial populations in the premature infant gut. Proc Natl Acad Sci U S A. 2014;111(34): 12522–12527. doi: 10.1073/pnas.1409497111
41. Mammas IN, Spandidos DA. Retinopathy of prematurity and neonatal gut microbiome: An interview with Professor Dimitra Skondra, Associate Professor of Ophthalmology and Vitreoretinal Surgeon at The University of Chicago (USA). Exp Ther Med. 2020;20(6): 294. doi: 10.3892/etm.2020.9424
42. Claud EC, Walker WA. Hypothesis: inappropriate colonization of the premature intestine can cause neonatal necrotizing enterocolitis. FASEB J. 2001;15(8): 1398–1403. doi: 10.1096/fj.00-0833hyp
43. Wang Y, Hoenig JD, Malin KJ, Qamar S, Petrof EO, Sun J, Antonopoulos DA, Chang EB, Claud EC. 16S rRNA gene-based analysis of fecal microbiota from preterm infants with and without necrotizing enterocolitis. ISME J. 2009;3(8): 944–954. doi: 10.1038/ismej.2009.37
44. Torrazza RM, Ukhanova M, Wang X, Sharma R, Hudak ML, Neu J, Mai V. Intestinal microbial ecology and environmental factors affecting necrotizing enterocolitis. PLoS One. 2013;8(12): e83304. doi: 10.1371/journal.pone.0083304
45. Warner BB, Deych E, Zhou Y, Hall-Moore C, Weinstock GM, Sodergren E, Shaikh N, Hoffmann JA, Linneman LA, Hamvas A, Khanna G, Rouggly-Nickless LC, Ndao IM, Shands BA, Escobedo M, Sullivan JE, Radmacher PG, Shannon WD, Tarr PI. Gut bacteria dysbiosis and necrotising enterocolitis in very low birthweight infants: a prospective case-control study. Lancet. 2016;387(10031): 1928–1936. doi: 10.1016/S0140-6736(16)00081-7
46. Pammi M, Cope J, Tarr PI, Warner BB, Morrow AL, Mai V, Gregory KE, Kroll JS, McMurtry V, Ferris MJ, Engstrand L, Lilja HE, Hollister EB, Versalovic J, Neu J. Intestinal dysbiosis in preterm infants preceding necrotizing enterocolitis: a systematic review and meta-analysis. Microbiome. 2017;5(1): 31. doi: 10.1186/s40168-017-0248-8
47. Scuderi G, Troiani E, Minnella AM. Gut Microbiome in Retina Health: The Crucial Role of the Gut-Retina Axis. Front Microbiol. 2022;12: 726792. doi: 10.3389/fmicb.2021.726792
48. Zysset-Burri DC, Morandi S, Herzog EL, Berger LE, Zinkernagel MS. The role of the gut microbiome in eye diseases. Prog Retin Eye Res. 2023;92: 101117. doi: 10.1016/j.preteyeres.2022.101117
49. Skondra D, Rodriguez SH, Sharma A, Gilbert J, Andrews B, Claud EC. The early gut microbiome could protect against severe retinopathy of prematurity. J AAPOS. 2020;24(4): 236–238. doi: 10.1016/j.jaapos.2020.03.010
50. Cane G, Moal VL, Pagès G, Servin AL, Hofman P, Vouret-Craviari V. Up-regulation of intestinal vascular endothelial growth factor by Afa/Dr diffusely adhering Escherichia coli. PLoS One. 2007;2(12): e1359. doi: 10.1371/journal.pone.0001359
51. Tran PM, Tang SS, Salgado-Pabón W. Staphylococcus aureus β-Toxin Exerts Anti-angiogenic Effects by Inhibiting Re-endothelialization and Neovessel Formation. Front Microbiol. 2022;13: 840236. doi: 10.3389/fmicb.2022.840236
52. Westaway JAF, Huerlimann R, Kandasamy Y, Miller CM, Norton R, Staunton KM, Watson D, Rudd D. The bacterial gut microbiome of probiotic-treated very-preterm infants: changes from admission to discharge. Pediatr Res. 2022;92(1): 142–150. doi: 10.1038/s41390-021-01738-6
53. Yan J, Herzog JW, Tsang K, Brennan CA, Bower MA, Garrett WS, Sartor BR, Aliprantis AO, Charles JF. Gut microbiota induce IGF-1 and promote bone formation and growth. Proc Natl Acad Sci U S A. 2016;113(47): E7554–E7563. doi: 10.1073/pnas.1607235113
54. Lee CC, Feng Y, Yeh YM, Lien R, Chen CL, Zhou YL, Chiu CH. Gut Dysbiosis, Bacterial Colonization and Translocation, and Neonatal Sepsis in Very-Low-Birth-Weight Preterm Infants. Front Microbiol. 2021;12: 746111. doi: 10.3389/fmicb.2021.746111
55. Frazer LC, Yakah W, Martin CR. Decreased Acetic Acid in the Stool of Preterm Infants Is Associated with an Increased Risk of Bronchopulmonary Dysplasia. Nutrients. 2022;14(12): 2412. doi: 10.3390/nu14122412
56. Schreiner C, Müller A, Dresbach T. Microbiological Screening of Donor Human Milk. Breastfeed Med. 2023;18(12): 901-907. doi: 10.1089/bfm.2023.0155
57. Kim ES, Calkins KL, Chu A. Retinopathy of Prematurity: The Role of Nutrition. Pediatr Ann. 2023;52(8): 303–308. doi: 10.3928/19382359 20230613-06
58. Walsh C, Lane JA, van Sinderen D, Hickey RM. Human milk oligosaccharides: Shaping the infant gut microbiota and supporting health. J Funct Foods. 2020;72: 104074. doi: 10.1016/j.jff.2020.104074
59. Bai WH, Gu DF, Dai Y, Chen YH, Yang ZM, Lu LJ. The relationship between probiotics and retinopathy of prematurity in preterm infants: A population-based retrospective study in China. Front Pediatr. 2023;11: 1055992. doi: 10.3389/fped.2023.1055992
60. Cavallaro G, Villamor-Martínez E, Filippi L, Mosca F, Villamor E. Probiotic supplementation in preterm infants does not affect the risk of retinopathy of prematurity: a meta-analysis of randomized controlled trials. Sci Rep. 2017;7(1): 13014. doi: 10.1038/s41598-017-13465-2